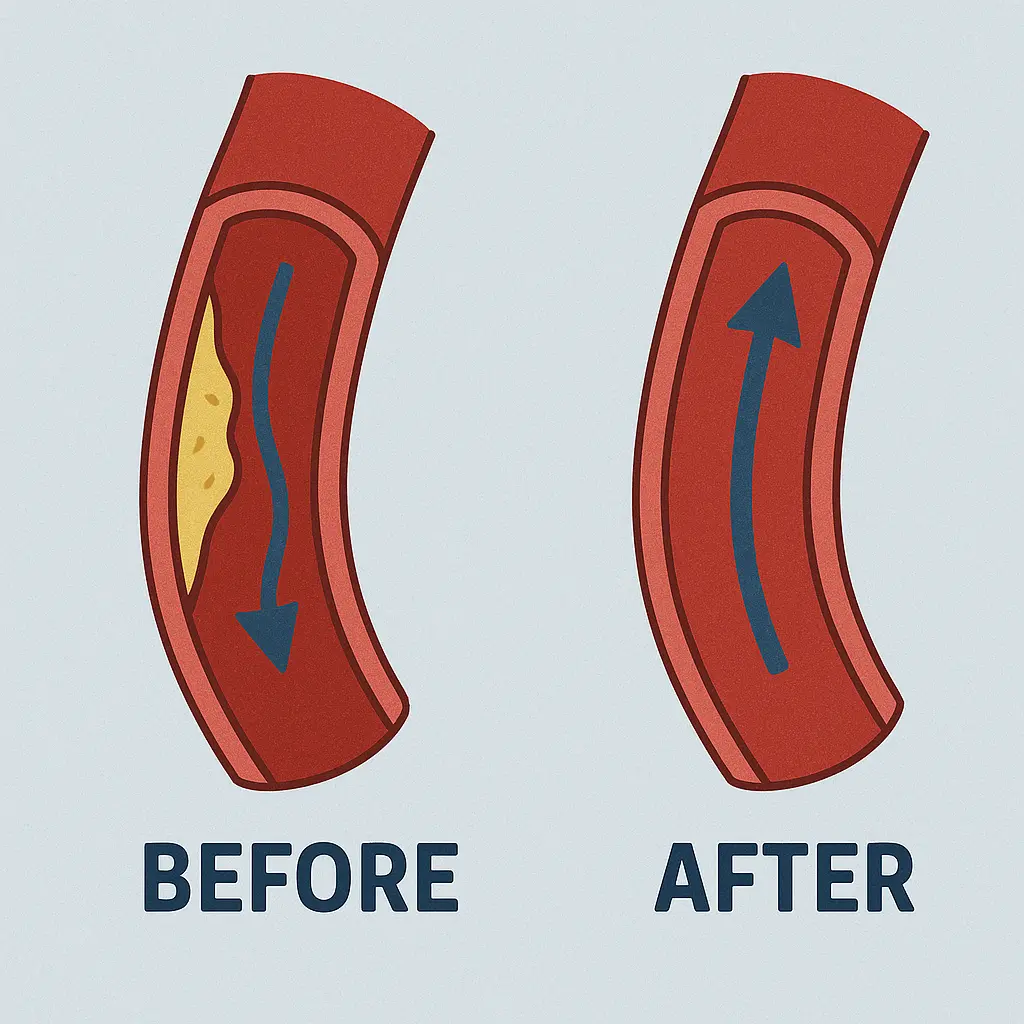
Atherectomy is a minimally invasive medical procedure used to remove plaque buildup from inside the arteries. Unlike angioplasty, which pushes plaque against artery walls, atherectomy actually removes it — helping restore proper blood flow. This treatment is often used in patients with:
- Peripheral artery disease (PAD)
- Coronary artery disease (CAD)
- Severely calcified or hardened arteries
If the term sounds unfamiliar, don’t worry — this guide explains how atherectomy works, its benefits, and what to expect.
How Does Atherectomy Work?
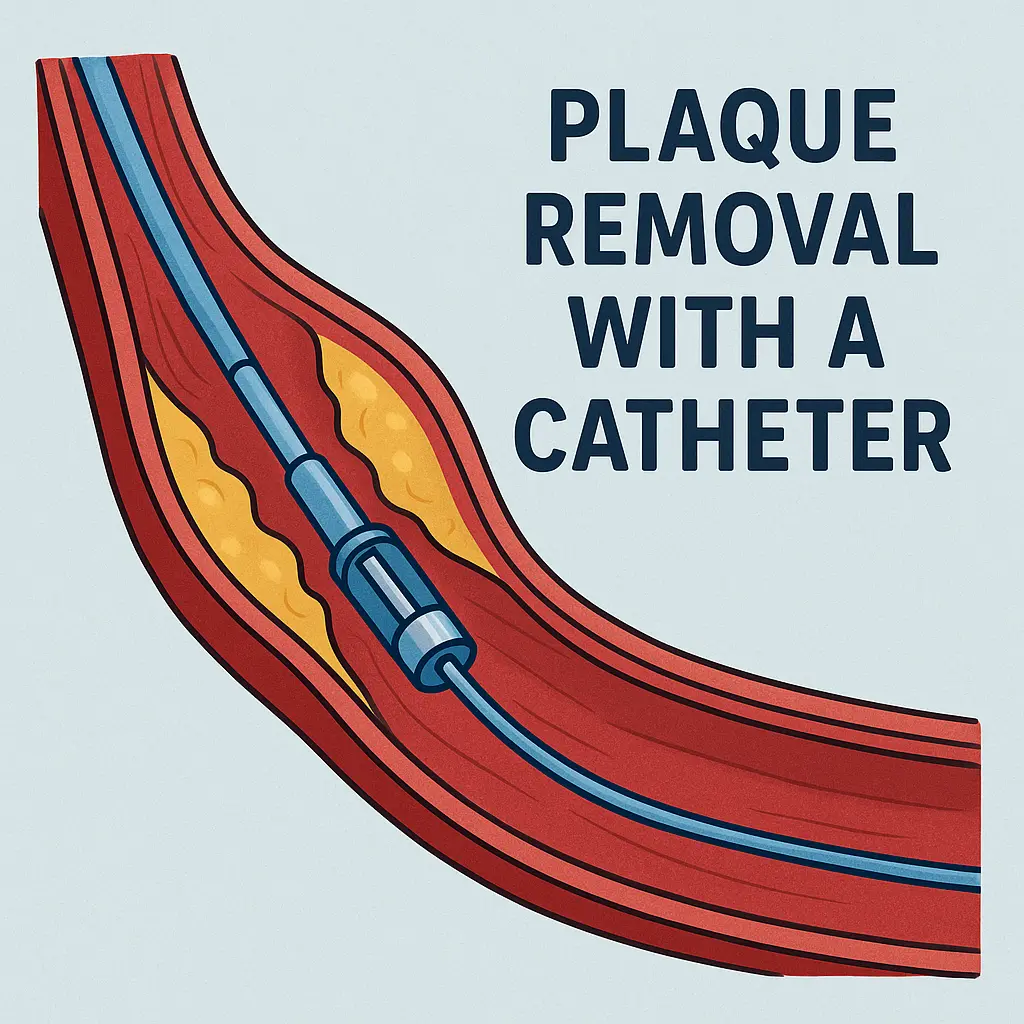
Here’s a simplified step-by-step overview of what typically happens during the procedure:
- Local anesthetic is applied to numb the area.
- A small incision is made, usually in the groin or wrist.
- A catheter (thin tube) is inserted into the artery.
- The catheter is guided to the blockage site.
- A specialized tool removes or breaks up the plaque.
- The catheter is withdrawn, and the incision is closed — often without stitches.
Procedure Time: 1 to 2 hours
Hospital Stay: Usually outpatient or 1 night
Recovery: Minimal downtime
Why is Atherectomy Performed?
Atherectomy is often chosen when:
- Plaque is hard or calcified, making angioplasty less effective
- Arteries are narrow, curved, or difficult to reach with stents
- Previous angioplasty or stenting was unsuccessful
- Open surgery poses too high a risk for the patient
In summary, atherectomy is a suitable option for treating complex artery blockages, especially in the legs or heart.
Types of Atherectomy Devices
There are four main types of devices used, depending on the situation:
| Type | How It Works | Best For |
|---|---|---|
| Directional | Uses a blade to shave plaque in one direction | Large, localized blockages |
| Rotational | High-speed drill removes hard plaque | Calcified coronary arteries |
| Orbital | Spinning crown sands plaque off | Narrow, curved vessels |
| Laser | Vaporizes plaque using light energy | Delicate or unreachable areas |
The choice of device depends on your artery type and the nature of the plaque.
Benefits of Atherectomy
- Physically removes plaque, unlike balloon angioplasty
- May reduce the need for stents or bypass surgery
- Short recovery period with low complication rate
- Can be repeated if blockages return
- Well-suited for patients with other medical conditions
Risks and Side Effects
Although generally safe, potential risks include:
- Bleeding or bruising at the incision site
- Damage to the blood vessel
- Plaque fragments traveling downstream (embolization)
- Infection (rare)
- Allergic reaction to contrast dye used in imaging
Your healthcare team monitors and manages these risks during the procedure.
Recovery and Aftercare
Most people resume normal activity within a week or two. A typical recovery timeline:
| Timeframe | What to Expect |
|---|---|
| First 24 hours | Rest, avoid strenuous movement, monitor incision |
| 2–3 days | Light walking is encouraged |
| Week 1–2 | Return to most regular activities |
| Ongoing | Lifestyle management and follow-up care |
Tip: A daily walking routine improves circulation and recovery outcomes. You may explore options like walking vs running for cardiovascular fitness and weight management.
Comparing Atherectomy, Angioplasty, and Stenting
| Feature | Atherectomy | Angioplasty | Stenting |
|---|---|---|---|
| Removes plaque | ✔ | ✘ | ✘ |
| Uses foreign object | ✘ (optional) | ✘ | ✔ (stent) |
| Good for calcified plaque | ✔ | ✘ | ✔ (sometimes) |
| Risk of re-narrowing | Low | Moderate | Moderate |
Integrating Atherectomy with Holistic Health
While atherectomy addresses the mechanical blockage, holistic health habits play a critical role in long-term success. Regular movement, plant-forward diets, stress reduction, and even therapeutic techniques like hydrotherapy can support your vascular system. Practices such as cold plunge therapy have been shown to improve circulation and reduce inflammation — key contributors to cardiovascular health. However, always consult your healthcare provider before incorporating such therapies into your post-procedure routine.
Who Is a Good Candidate for Atherectomy?
Not every patient with artery disease is suited for atherectomy. It’s best considered when plaque is hard, eccentric, or not easily managed through balloon angioplasty or stenting alone. Ideal candidates include:
- Individuals with calcified plaque that resists traditional balloon expansion
- Patients who previously had unsuccessful angioplasty or stenting
- Those with small or tortuous vessels where stent placement is difficult
- Patients with high surgical risk who cannot undergo open bypass surgery
Before recommending this procedure, vascular specialists evaluate your imaging results, symptoms, and overall health condition to ensure atherectomy is the most effective and safe approach.
Preparing for Your Atherectomy Procedure
Proper preparation plays a vital role in reducing complications and improving outcomes. Your healthcare provider may advise the following steps:
- Undergo blood tests, EKG, and imaging (like angiography) to map the plaque location
- Adjust medications — particularly blood thinners, diabetes medications, and aspirin
- Stop eating or drinking for several hours before the procedure
- Arrange transportation and post-procedure assistance, as sedation is commonly used
Be transparent about any allergies (especially to contrast dye or iodine) or past surgical complications. You’ll receive detailed pre-op and post-op instructions tailored to your health status.
Long-Term Outlook and Lifestyle Adjustments
The long-term success of atherectomy largely depends on post-procedure lifestyle habits. While the physical plaque is removed, vascular disease is a chronic condition that requires ongoing care. To help prevent re-narrowing:
- Adopt a heart-healthy diet low in saturated fats and processed sugar
- Engage in regular aerobic activity — walking, swimming, or even moderate cycling
- Stop smoking and limit alcohol intake
- Manage blood pressure, cholesterol, and blood sugar levels with medication and lifestyle changes
Many patients benefit from joining cardiac rehabilitation programs or working with a nutritionist and fitness coach. Building healthy habits not only supports better outcomes but also enhances overall quality of life.

Cost of Atherectomy in the U.S.
The average cost ranges from $10,000 to $25,000 depending on location and complexity. Most insurance plans — including Medicare — cover it when deemed medically necessary.
Tip: Always request a detailed estimate from your provider before the procedure.
Frequently Asked Questions
- 1. Is atherectomy painful?
- No. The procedure uses local anesthesia, and most patients feel little to no pain.
- 2. Will I need a stent afterward?
- Not always. In some cases, plaque removal is enough. If the artery risks collapsing, a stent may be inserted.
- 3. How long do the effects last?
- Results vary by patient. Healthy lifestyle changes — like walking and quitting smoking — extend the benefits.
- 4. Can the procedure be repeated?
- Yes, atherectomy can be performed again if necessary.
- 5. Is it better than bypass surgery?
- For many, yes. Atherectomy is far less invasive and quicker to recover from, though bypass may still be needed in some cases.
External Resources
- American Heart Association – Coronary Artery Disease
- Society for Vascular Surgery – PAD Resource Center
Conclusion
If you’re dealing with blocked arteries, poor circulation, or have had limited success with other treatments, atherectomy may be a safe and effective option. It removes plaque rather than just compressing it, often helping avoid more invasive surgeries. Combined with lifestyle strategies like walking and proper dietary care, the benefits can be long-lasting. Discuss your options with a vascular specialist to determine the best path forward.